Remitió Ruben Piacentini.
It’s not edible, but it can save lives. The virologist Ian Mackay explains how.
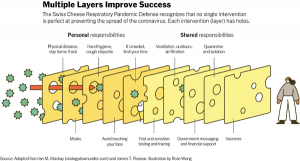
Lately, in the ongoing conversation about how to defeat the coronavirus, experts have made reference to the “Swiss cheese model” of pandemic defense.
The metaphor is easy enough to grasp: Multiple layers of protection, imagined as cheese slices, block the spread of the new coronavirus, SARS-CoV-2, the virus that causes Covid-19. No one layer is perfect; each has holes, and when the holes align, the risk of infection increases. But several layers combined — social distancing, plus masks, plus hand-washing, plus testing and tracing, plus ventilation, plus government messaging — significantly reduce the overall risk. Vaccination will add one more protective layer.
“Pretty soon you’ve created an impenetrable barrier, and you really can quench the transmission of the virus,” said Dr. Julie Gerberding, executive vice president and chief patient officer at Merck, who recently referenced the Swiss cheese model when speaking at a virtual gala fund-raiser for MoMath, the National Museum of Mathematics in Manhattan.
“But it requires all of those things, not just one of those things,” she added. “I think that’s what our population is having trouble getting their head around. We want to believe that there is going to come this magic day when suddenly 300 million doses of vaccine will be available and we can go back to work and things will return to normal. That is absolutely not going to happen fast.”
Rather, Dr. Gerberding said in a follow-up email, expect to see “a gradual improvement in protection, first among the highest need groups, and then more gradually among the rest of us.” Until vaccines are widely available and taken, she said, “we will need to continue masks and other common-sense measures to protect ourselves and others.”
In October, Bill Hanage, an epidemiologist at the Harvard T.H. Chan School of Public Health, retweeted an infographic rendering of the Swiss cheese model, noting that it included “things that are personal *and* collective responsibility — note the ‘misinformation mouse’ busy eating new holes for the virus to pass through.”
“One of the first principles of pandemic response is, or ought to be, clear and consistent messaging from trusted sources,” Dr. Hanage said in an email. “Unfortunately the independence of established authorities like the C.D.C. has been called into question, and trust needs to be rebuilt as a matter of urgency.” A catchy infographic is a powerful message, he said, but ultimately requires higher-level support.
The Swiss cheese concept originated with James T. Reason, a cognitive psychologist, now a professor emeritus at the University of Manchester, England, in his 1990 book, “Human Error.” A succession of disasters — including the Challenger shuttle explosion, Bhopal and Chernobyl — motivated the concept, and it became known as the “Swiss cheese model of accidents,” with the holes in the cheese slices representing errors that accumulate and lead to adverse events.
The model has been widely used by safety analysts in various industries, including medicine and aviation, for many years. (Dr. Reason did not devise the “Swiss cheese” label; that is attributed to Rob Lee, an Australian air-safety expert, in the 1990s.) The model became famous, but it was not accepted uncritically; Dr. Reason himself noted that it had limitations and was intended as a generic tool or guide. In 2004, at a workshop addressing an aviation accident two years earlier near Überlingen, Germany, he delivered a talk with the title, “Überlingen: Is Swiss cheese past its sell-by date?”
In 2006, a review of the model, published by the Eurocontrol Experimental Center, recounted that Dr. Reason, while writing the book chapter “Latent errors and system disasters,” in which an early version of the model appears, was guided by two notions: “the biological or medical metaphor of pathogens, and the central role played by defenses, barriers, controls and safeguards (analogous to the body’s autoimmune system).”
The cheese metaphor now pairs fairly well with the coronavirus pandemic. Ian M. Mackay, a virologist at the University of Queensland, in Brisbane, Australia, saw a smaller version on Twitter, but thought that it could do with more slices, more information. He created, with collaborators, the “Swiss Cheese Respiratory Pandemic Defense” and engaged his Twitter community, asking for feedback and putting the visualization through many iterations. “Community engagement is very high!” he said. Now circulating widely, the infographic has been translated into more than two dozen languages.

Dr. Mackay, a creator of the “Swiss Cheese Respiratory Pandemic Defense.”Credit…Faye Sakura for The New York Times
“This multilayered approach to reducing risk is used in many industries, especially those where failure could be catastrophic,” Dr. Mackay said, via email. “Death is catastrophic to families, and for loved ones, so I thought Professor Reason’s approach fit in very well during the circulation of a brand-new, occasionally hidden, sometimes severe and occasionally deadly respiratory virus.”
The following is an edited version of a recent email conversation with Dr. Mackay.
Q. What does the Swiss cheese model show?
The real power of this infographic — and James Reason’s approach to account for human fallibility — is that it’s not really about any single layer of protection or the order of them, but about the additive success of using multiple layers, or cheese slices. Each slice has holes or failings, and those holes can change in number and size and location, depending on how we behave in response to each intervention.
Take masks as one example of a layer. Any mask will reduce the risk that you will unknowingly infect those around you, or that you will inhale enough virus to become infected. But it will be less effective at protecting you and others if it doesn’t fit well, if you wear it below your nose, if it’s only a single piece of cloth, if the cloth is a loose weave, if it has an unfiltered valve, if you don’t dispose of it properly, if you don’t wash it, or if you don’t sanitize your hands after you touch it. Each of these are examples of a hole. And that’s in just one layer.
To be as safe as possible, and to keep those around you safe, it’s important to use more slices to prevent those volatile holes from aligning and letting virus through.
Q. What have we learned since March?
Distance is the most effective intervention; the virus doesn’t have legs, so if you are physically distant from people, you avoid direct contact and droplets. Then you have to consider inside spaces, which are especially in play during winter or in hotter countries during summer: the bus, the gym, the office, the bar or the restaurant. That’s because we know SARS-CoV-2 can remain infectious in aerosols (small floaty droplets) and we know that aerosol spread explains Covid-19 superspreading events. Try not to be in those spaces with others, but if you have to be, minimize your time there (work from home if you can) and wear a mask. Don’t go grocery shopping as often. Hold off on going out, parties, gatherings. You can do these things later.
The Road to a Coronavirus Vaccine
Words to Know About Vaccines
Confused by the all technical terms used to describe how vaccines work and are investigated? Let us help:
- Adverse event: A health problem that crops up in volunteers in a clinical trial of a vaccine or a drug. An adverse event isn’t always caused by the treatment tested in the trial.
- Antibody: A protein produced by the immune system that can attach to a pathogen such as the coronavirus and stop it from infecting cells.
- Approval, licensure and emergency use authorization: Drugs, vaccines and medical devices cannot be sold in the United States without gaining approval from the Food and Drug Administration, also known as licensure. After a company submits the results of clinical trials to the F.D.A. for consideration, the agency decides whether the product is safe and effective, a process that generally takes many months. If the country is facing an emergency — like a pandemic — a company may apply instead for an emergency use authorization, which can be granted considerably faster.
- Background rate: How often a health problem, known as an adverse event, arises in the general population. To determine if a vaccine or a drug is safe, researchers compare the rate of adverse events in a trial to the background rate.
- Efficacy: The benefit that a vaccine provides compared to a placebo, as measured in a clinical trial. To test a coronavirus vaccine, for instance, researchers compare how many people in the vaccinated and placebo groups get Covid-19. Effectiveness, by contrast, is the benefit that a vaccine or a drug provides out in the real world. A vaccine’s effectiveness may turn out to be lower or higher than its efficacy.
- Phase 1, 2, and 3 trials: Clinical trials typically take place in three stages. Phase 1 trials usually involve a few dozen people and are designed to observe whether a vaccine or drug is safe. Phase 2 trials, involving hundreds of people, allow researchers to try out different doses and gather more measurements about the vaccine’s effects on the immune system. Phase 3 trials, involving thousands or tens of thousands of volunteers, determine the safety and efficacy of the vaccine or drug by waiting to see how many people are protected from the disease it’s designed to fight.
- Placebo: A substance that has no therapeutic effect, often used in a clinical trial. To see if a vaccine can prevent Covid-19, for example, researchers may inject the vaccine into half of their volunteers, while the other half get a placebo of salt water. They can then compare how many people in each group get infected.
- Post-market surveillance: The monitoring that takes place after a vaccine or drug has been approved and is regularly prescribed by doctors. This surveillance typically confirms that the treatment is safe. On rare occasions, it detects side effects in certain groups of people that were missed during clinical trials.
- Preclinical research: Studies that take place before the start of a clinical trial, typically involving experiments where a treatment is tested on cells or in animals.
- Viral vector vaccines: A type of vaccine that uses a harmless virus to chauffeur immune-system-stimulating ingredients into the human body. Viral vectors are used in several experimental Covid-19 vaccines, including those developed by AstraZeneca and Johnson & Johnson. Both of these companies are using a common cold virus called an adenovirus as their vector. The adenovirus carries coronavirus genes.
- Trial protocol: A series of procedures to be carried out during a clinical trial.
We don’t talk about eye coverings much, but we should, because we don’t know enough about the role of eyes in transmission. We do know that eyes are a window to the upper respiratory tract.
Q. Where does the “misinformation mouse” fit in?
The misinformation mouse can erode any of those layers. People who are uncertain about an intervention may be swayed by a loud and confident-sounding voice proclaiming that a particular layer is ineffective. Usually, that voice is not an expert on the subject at all. When you look to the experts — usually to your local public health authorities or the World Health Organization — you’ll find reliable information.
An effect doesn’t have to be perfect to reduce your risk and the risk to those around you. We need to remember that we’re all part of a society, and if we each do our part, we can keep each other safer, which pays off for us as well.
Another example: We look both ways for oncoming traffic before crossing a road. This reduces our risk of being hit by a car but doesn’t reduce it to zero. A speeding car could still come out of nowhere. But if we also cross with the lights, and keep looking as we walk, and don’t stare at our phone, we drastically reduce our risk of being hit.
We’re already used to doing that. When we listen to the loud nonexperts who have no experience in protecting our health and safety, we are inviting them to have an impact in our lives. That’s not a risk we should take. We just need to get used to these new risk-reduction steps for today’s new risk — a respiratory virus pandemic, instead of a car.
Q. What is our individual responsibility?
We each need to do our part: stay apart from others, wear a mask when we can’t, think about our surroundings, for example. But we can also expect our leadership to be working to create the circumstances for us to be safe — like regulations about the air exchange inside public spaces, creating quarantine and isolation premises, communicating specifically with us (not just at us), limiting border travel, pushing us to keep getting our health checks, and providing mental health or financial support for those who suffer or can’t get paid while in a lockdown.
Q. How can we make the model stick?
We each use these approaches in everyday life. But for the pandemic, this all feels new and like a lot of extra work. Because everything is new. In the end, though, we’re just forming new habits. Like navigating our latest phone’s operating system or learning how to play that new console game I got for my birthday. It might take some time to get across it all, but it’s worthwhile. In working together to reduce the risk of infection, we can save lives and improve health.
And as a bonus, the multilayered risk reduction approach can even decrease the number of times we get the flu or a bad chest cold. Also, sometimes slices sit under a mandate — it’s important we also abide by those rules and do what the experts think we should. They’re looking out for our health.
